Abstract
Background
Myocardial injury is frequent among patients hospitalized with coronavirus disease-2019 (COVID-19) and is associated with a poor prognosis. However, the mechanisms of myocardial injury remain unclear and prior studies have not reported cardiovascular imaging data.
Objectives
This study sought to characterize the echocardiographic abnormalities associated with myocardial injury and their prognostic impact in patients with COVID-19.
Methods
We conducted an international, multicenter cohort study including 7 hospitals in New York City and Milan of hospitalized patients with laboratory-confirmed COVID-19 who had undergone transthoracic echocardiographic (TTE) and electrocardiographic evaluation during their index hospitalization. Myocardial injury was defined as any elevation in cardiac troponin at the time of clinical presentation or during the hospitalization.
Results
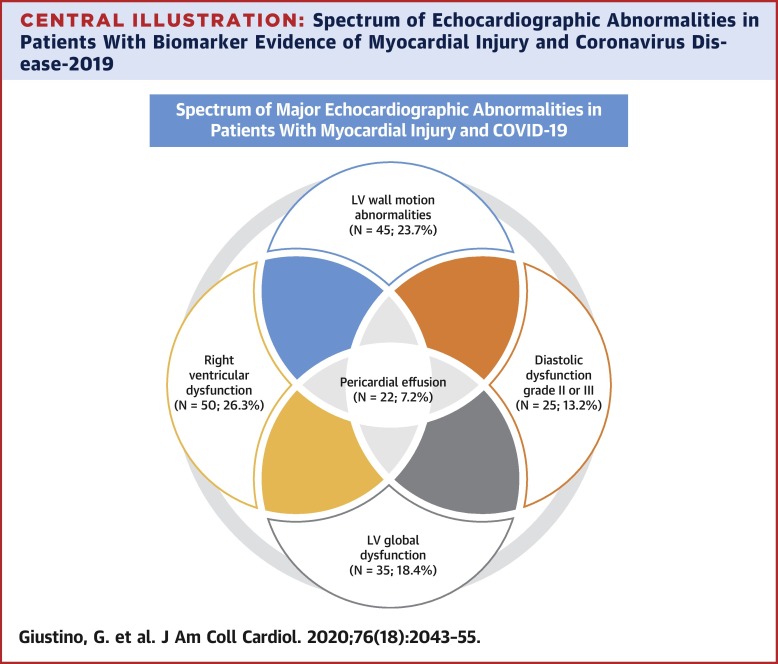
A total of 305 patients were included. Mean age was 63 years and 205 patients (67.2%) were male. Overall, myocardial injury was observed in 190 patients (62.3%). Compared with patients without myocardial injury, those with myocardial injury had more electrocardiographic abnormalities, higher inflammatory biomarkers and an increased prevalence of major echocardiographic abnormalities that included left ventricular wall motion abnormalities, global left ventricular dysfunction, left ventricular diastolic dysfunction grade II or III, right ventricular dysfunction and pericardial effusions. Rates of in-hospital mortality were 5.2%, 18.6%, and 31.7% in patients without myocardial injury, with myocardial injury without TTE abnormalities, and with myocardial injury and TTE abnormalities. Following multivariable adjustment, myocardial injury with TTE abnormalities was associated with higher risk of death but not myocardial injury without TTE abnormalities.
Conclusions
Among patients with COVID-19 who underwent TTE, cardiac structural abnormalities were present in nearly two-thirds of patients with myocardial injury. Myocardial injury was associated with increased in-hospital mortality particularly if echocardiographic abnormalities were present.