Realities, challenges and development levers
Auteur/autrice : Taha-Sefiani
The year in cardiovascular medicine 2020, articles sélectionnés par Dr Tahar El Kandoussi. El Hoceima
Peripartum management of hypertension: a position paper of the ESC Council on Hypertension and the European Society of Hypertension
Abstract :
Hypertensive disorders are the most common medical complications in the peripartum period associated with a substantial increase in morbidity and mortality. Hypertension in the peripartum period may be due to the continuation of pre-existing or gestational hypertension, de novo development of pre-eclampsia or it may be also induced by some drugs used for analgesia or suppression of postpartum haemorrhage. Women with severe hypertension and hypertensive emergencies are at high risk of life-threatening complications, therefore, despite the lack of evidence-based data, based on expert opinion, antihypertensive treatment is recommended. Labetalol intravenously and methyldopa orally are then the two most frequently used drugs. Short-acting oral nifedipine is suggested to be used only if other drugs or iv access are not available. Induction of labour is associated with improved maternal outcome and should be advised for women with gestational hypertension or mild pre-eclampsia at 37 weeks’ gestation. This position paper provides the first interdisciplinary approach to the management of hypertension in the peripartum period based on the best available evidence and expert consensus.
Quoi de neuf en insuffisance cardiaque?
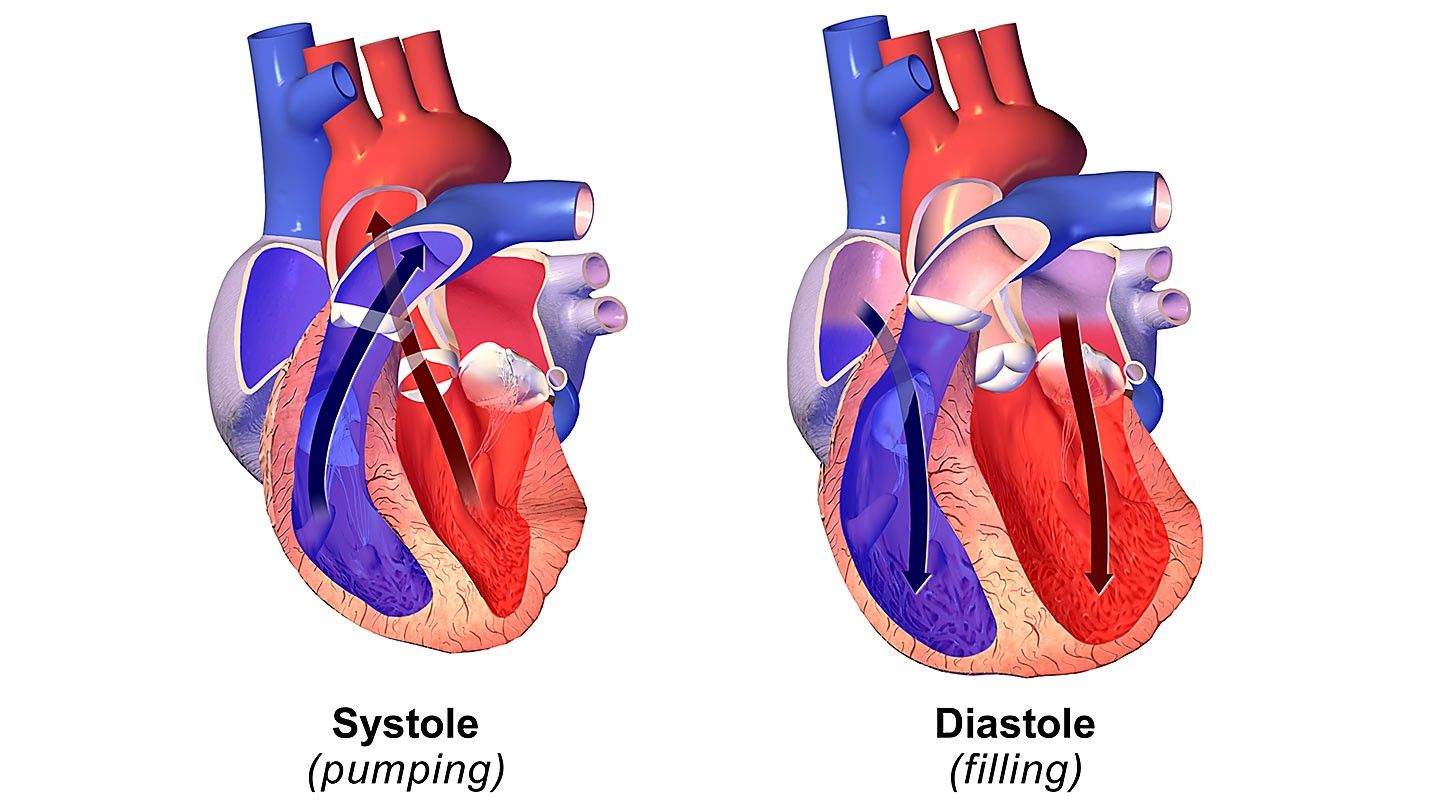
Les inégalités thérapeutiques dans la prise en charge des insuffisances cardiaques à fraction d’éjection réduite (ICFEr) et préservée (ICFEp) continuent à se creuser. En effet, ces 12 derniers mois, deux nouvelles classes thérapeutiques [1, 2], les inhibiteurs sélectifs du cotransporteur 2 du sodium- glucose (SGLT2) et les stimulateurs de la guanylate cyclase soluble (GCs), se sont révélées efficaces dans le traite- ment de l’ICFEr. Ces résultats amènent à réfléchir sur la place respective de ces traitements dans l’algorithme théra- peutique de cette maladie qui semblait gravé dans le marbre depuis les dernières recommandations de 2016 [3], alors que le plus grand essai thérapeutique jamais réalisé en matière de traitement de l’ICFEp, l’étude PARAGON-HF avec le sacubitril-valsartan [4] s’est révélé une nouvelle fois neutre, soulignant les limites du traitement de cette patholo- gie pléiotrope, complexe, qui intéresse pourtant 50 % de nos patients.
An Electronically Delivered, Patient-Activation Tool for Intensification of Medications for Chronic Heart Failure with Reduced Ejection Fraction: The EPIC-HF Trial
A randomized clinical trial of early invasive intervention for atrial fibrillation (EARLY-AF) – methods and rationale
Ticagrelor Added to Aspirin in Acute Ischemic Stroke or Transient Ischemic Attack in Prevention of Disabling Stroke : A Randomized Clinical Trial
N-of-1 Trial of a Statin, Placebo, or No Treatment to Assess Side Effects
Cardiac Myosin Activation with Omecamtiv Mecarbil in Systolic Heart Failure
Vital capacity and COPD: the swedish CardioPulmonary bioImage study (sCaPIs)
Abstract
Background
Spirometric diagnosis of chronic obstructive pulmonary disease (COPD) is based on the ratio of forced expiratory volume in 1 second (FEV )/vital capacity (VC), either as a fixed value <0.7 or below the lower limit of normal (LLN). Forced vital capacity (FVC) is a proxy for VC. The first aim was to compare the use of FVC and VC, assessed as the highest value of FVC or slow vital capacity (SVC), when assessing the FEV1/VC ratio in a general population setting. The second aim was to evaluate the characteristics of subjects with COPD who obtained a higher SVC than FVC.
Methods
Subjects (n=1,050) aged 50–64 years were investigated with FEV1, FVC, and SVC after bronchodilation. Global Initiative for Chronic Obstructive Lung Disease (GOLD) COPDFVC was defined as FEV1/FVC ,0.7, GOLDCOPDVC as FEV1/VC ,0.7 using the maximum value of FVC or SVC, LLNCOPDFVC as FEV1/FVC below the LLN, and LLNCOPDVC as FEV1/VC below the LLN using the maximum value of FVC or SVC.
Results
Prevalence of GOLDCOPD FVC was 10.0% (95% confidence interval [CI] 8.2–12.0) and the prevalence of LLNCOPD FVC was 9.5% (95% CI 7.8–11.4). When estimates were based on VC, the prevalence became higher; 16.4% (95% CI 14.3–18.9) and 15.6% (95% CI 13.5–17.9) for GOLDCOPD VC and LLNCOPD VC, respectively. The group of additional subjects classified as having COPD based on VC, had lower FEV 1, more wheeze and higher residual volume
compared to subjects without any COPD.
Conclusions
The prevalence of COPD was significantly higher when the ratio FEV1 /VC was calculated using the highest value of SVC or FVC compared with using FVC only. Subjects classified as having COPD when using the VC concept were more obstructive and with indica- tions of air trapping. Hence, the use of only FVC when assessing airflow limitation may result in a considerable under diagnosis of subjects with mild COPD.