Catégorie : Général
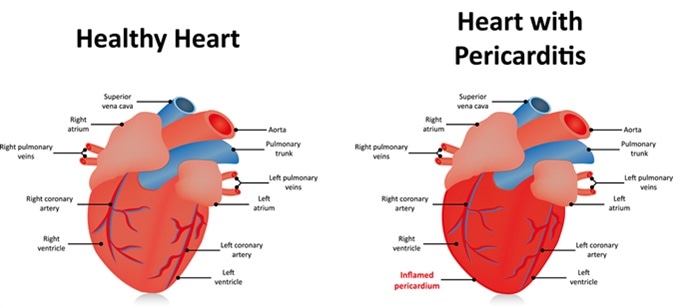
RHAPSODY : Rilonacept, an IL-1α and IL-1β, Resolves Pericarditis Episodes and reduces Risk of Recurrence in a phase 3 Trial of patients with Recurrent Pericarditis
Prise en charge des patients suspects ou confirmés COVID-19 en unités d’hospitalisation (y compris les unités de soins intensifs des urgences et la réanimation) – Version Novembre 2020
Auteurs :
Lahcen Belyamani, Ahmed Rhassane El Adib, Saïd Jidane, Jamaleddine Kohen, Abderrahim Azzouzi, Taoufik Aboulhassan, Saad Zidouh, Sifeddine Nejmi, Hicham Bakkali, Chafik Kettani, Mostapha Bensghir, Abdelhamid El Bait, Mamoun Faroudy, Ali Kettani, Afak Nsiri, Saïd Younous, Nabil Kanjaa, Adnane Berdai, Mustapha Abarda, Alae El Koraichi, Hicham Belkhi, Naoufal Madani, Brahim Housni, Karim Filali, Mohamed Mouhaoui, Nabil Kenjaa, Hanane Ezzouine, Youness El Aissaoui, Mohamed Nasser Semkaoui, Ismael Labib, Hicham Sbai, Mohamed Khatouf, Yassir Sbai, Abdelhamid Hachimi, Khalid Abidi, Saloua Marzak.
Les volets traités dans ces recommandations d’experts sont les suivants :
- Modalités de l’oxygénothérapie en fonction des moyens disponibles ;
- Modalités de prescription de l’acide acétylsalicylique ;
- Traitement anticoagulant ;
- Corticothérapie ;
- Traitements antiviraux ;
- Traitement anti-interleukine 6 ;
- Antibiothérapie et COVID ;
- Place du plasma de convalescents ;
- Sortie et suivi ambulatoire.
Registry of Arterial and Venous Thromboembolic Complications in Patients With COVID-19
Abstract
Background
Cardiovascular complications, including myocardial infarction, ischemic stroke, and pulmonary embo- lism, represent an important source of adverse outcomes in coronavirus disease-2019 (COVID-19).
Objectives
To assess the frequency of arterial and venous thromboembolic disease, risk factors, prevention and management patterns, and outcomes in patients with COVID-19, the authors designed a multicenter, observational cohort study.
Methods
We analyzed a retrospective cohort of 1,114 patients with COVID-19 diagnosed through our Mass General Brigham integrated health network. The total cohort was analyzed by site of care: intensive care (n 1⁄4 170); hospitalized nonintensive care (n 1⁄4 229); and outpatient (n 1⁄4 715). The primary study outcome was a composite of adjudicated major arterial or venous thromboembolism.
Results
Patients with COVID-19 were 22.3% Hispanic/Latinx and 44.2% non-White. Cardiovascular risk factors of hypertension (35.8%), hyperlipidemia (28.6%), and diabetes (18.0%) were common. Prophylactic anticoagulation was prescribed in 89.4% of patients with COVID-19 in the intensive care cohort and 84.7% of those in the hospitalized nonintensive care setting. Frequencies of major arterial or venous thromboembolism, major cardiovascular adverse events, and symptomatic venous thromboembolism were highest in the intensive care cohort (35.3%, 45.9%, and 27.0 %, respectively) followed by the hospitalized nonintensive care cohort (2.6%, 6.1%, and 2.2%, respectively) and the outpatient cohort (0% for all).
Conclusions
Major arterial or venous thromboembolism, major adverse cardiovascular events, and symptomatic venous thromboembolism occurred with high frequency in patients with COVID-19, especially in the intensive care setting,despiteahighutilizationrateofthromboprophylaxis. (JAmCollCardiol2020;76:2060–72)©2020TheAuthors. Published by Elsevier on behalf of the American College of Cardiology Foundation. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
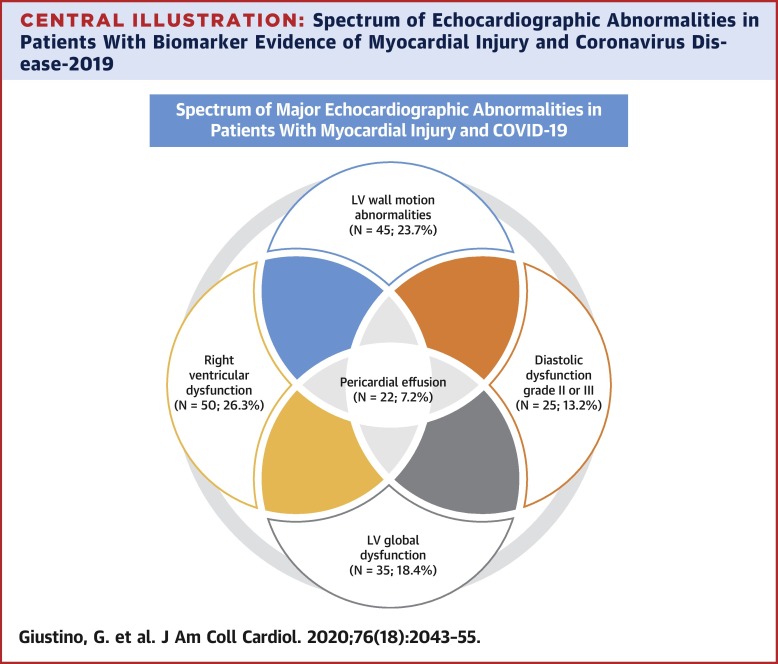
Characterization of Myocardial Injury in Patients With COVID-19
Abstract
Background
Myocardial injury is frequent among patients hospitalized with coronavirus disease-2019 (COVID-19) and is associated with a poor prognosis. However, the mechanisms of myocardial injury remain unclear and prior studies have not reported cardiovascular imaging data.
Objectives
This study sought to characterize the echocardiographic abnormalities associated with myocardial injury and their prognostic impact in patients with COVID-19.
Methods
We conducted an international, multicenter cohort study including 7 hospitals in New York City and Milan of hospitalized patients with laboratory-confirmed COVID-19 who had undergone transthoracic echocardiographic (TTE) and electrocardiographic evaluation during their index hospitalization. Myocardial injury was defined as any elevation in cardiac troponin at the time of clinical presentation or during the hospitalization.
Results
A total of 305 patients were included. Mean age was 63 years and 205 patients (67.2%) were male. Overall, myocardial injury was observed in 190 patients (62.3%). Compared with patients without myocardial injury, those with myocardial injury had more electrocardiographic abnormalities, higher inflammatory biomarkers and an increased prevalence of major echocardiographic abnormalities that included left ventricular wall motion abnormalities, global left ventricular dysfunction, left ventricular diastolic dysfunction grade II or III, right ventricular dysfunction and pericardial effusions. Rates of in-hospital mortality were 5.2%, 18.6%, and 31.7% in patients without myocardial injury, with myocardial injury without TTE abnormalities, and with myocardial injury and TTE abnormalities. Following multivariable adjustment, myocardial injury with TTE abnormalities was associated with higher risk of death but not myocardial injury without TTE abnormalities.
Conclusions
Among patients with COVID-19 who underwent TTE, cardiac structural abnormalities were present in nearly two-thirds of patients with myocardial injury. Myocardial injury was associated with increased in-hospital mortality particularly if echocardiographic abnormalities were present.
Remdesivir for the Treatment of Covid-19 — Final Report
Abstract
Background
Although several therapeutic agents have been evaluated for the treatment of coronavirus disease 2019 (Covid-19), no antiviral agents have yet been shown to be efficacious.
Methods
We conducted a double-blind, randomized, placebo-controlled trial of intravenous remdesivir in adults who were hospitalized with Covid-19 and had evidence of lower respiratory tract infection. Patients were randomly assigned to receive either remdesivir (200 mg loading dose on day 1, followed by 100 mg daily for up to 9 additional days) or placebo for up to 10 days. The primary outcome was the time to recovery, defined by either discharge from the hospital or hospitalization for infection-control purposes only.
Results
A total of 1062 patients underwent randomization (with 541 assigned to remdesivir and 521 to placebo). Those who received remdesivir had a median recovery time of 10 days (95% confidence interval [CI], 9 to 11), as compared with 15 days (95% CI, 13 to 18) among those who received placebo (rate ratio for recovery, 1.29; 95% CI, 1.12 to 1.49; P<0.001, by a log-rank test). In an analysis that used a proportional-odds model with an eight-category ordinal scale, the patients who received remdesivir were found to be more likely than those who received placebo to have clinical improvement at day 15 (odds ratio, 1.5; 95% CI, 1.2 to 1.9, after adjustment for actual disease severity). The Kaplan–Meier estimates of mortality were 6.7% with remdesivir and 11.9% with placebo by day 15 and 11.4% with remdesivir and 15.2% with placebo by day 29 (hazard ratio, 0.73; 95% CI, 0.52 to 1.03). Serious adverse events were reported in 131 of the 532 patients who received remdesivir (24.6%) and in 163 of the 516 patients who received placebo (31.6%).
Conclusions
Our data show that remdesivir was superior to placebo in shortening the time to recovery in adults who were hospitalized with Covid-19 and had evidence of lower respiratory tract infection. (Funded by the National Institute of Allergy and Infectious Diseases and others; ACTT-1 ClinicalTrials.gov number, NCT04280705. opens in new tab.)
SGLT2 inhibitors in patients with heart failure with reduced ejection fraction: a meta-analysis of the EMPEROR-Reduced and DAPA-HF trials
La Société marocaine de Cardiologie célèbre la journée mondiale du coeur
La Journée Mondiale du Cœur (WHD) est fixée au 29 septembre de chaque année : c’est le plus grand événement de la Fédération mondiale du cœur et du monde entier pour sensibiliser davantage les gens aux maladies cardiovasculaires, qui incluent les maladies cardiaques et les AVC.
Actualités ESC 2020: Essais et études – Articles réunis par le Dr Mohamed Ztati.
Timing of Intervention in Asymptomatic Patients With Valvular Heart Disease
Authors: Baumgartner H, Iung B, Otto CM.
Citation: Timing of Intervention in Asymptomatic Patients With Valvular Heart Disease. Eur Heart J 2020;Sep 9:[Epub ahead of print].
Current management recommendations for patients with valvular heart disease time intervention in an attempt to optimize long-term outcomes. The following are key points to remember from this review, which summarizes current recommendations for intervention in asymptomatic patients with heart valve disease and discusses more recently published data that might favor earlier intervention in some patients:
1.Weighing the risks and benefits for intervention in asymptomatic patients :
- Rationale for intervention in asymptomatic patients include the risk of life-threatening events in the absence of pre-existing symptoms, irreversible end-organ damage (particularly the left ventricle [LV] and pulmonary vasculature) despite the absence of symptoms, a lower risk associated with earlier intervention, insidious symptoms that might not be recognized, and avoiding problems with suboptimal follow-up or delayed intervention once an indication is recognized.
- The risks of intervention include operative risks and long-term risks after intervention.
- Variables to be weighed include the type of heart valve disease; the type of intervention; the strength of any predictors for adverse outcomes; and patient age, comorbidities, and general condition.
2.Aortic stenosis (AS) :
- Variables that have been associated with outcomes are derived from echocardiography, exercise testing, and biomarkers including B-type natriuretic peptide (BNP).
- Current American Heart Association/American College of Cardiology (AHA/ACC) and/or European Society of Cardiology/European Association for Cardio-Thoracic Surgery (ESC/EACTS) guidelines support intervention in asymptomatic patients with severe AS plus LV systolic dysfunction not due to another cause (variably LV ejection fraction [LVEF] ≤50% or <50%), abnormal exercise testing, or low surgical risk, and either very severe AS or rapid progression of AS.
- Several randomized clinical trials are underway testing early intervention in patients with asymptomatic AS.
- Published studies support the roles of myocardial fibrosis on cardiac magnetic resonance imaging, LVEF <55% or <60%, LV global longitudinal strain (GLS), and biomarkers in the assessment of AS outcomes.
3.Aortic regurgitation (AR) :
- Variables that have been associated with outcomes include LV enlargement and systolic dysfunction, BNP, and concomitant ascending aorta enlargement.
- Current AHA/ACC and/or ESC/EACTS guidelines support intervention in asymptomatic patients with severe AR plus LV systolic dysfunction (variably LVEF <50% or ≤50%), or severe LV dilation.
- Published studies support the roles of a lower threshold for LV dilation (LV end-systolic diameter index 20-25 mm/m2 rather than >25 mm/m2), LVEF <55%, or abnormal LV GLS in the assessment of AR outcomes.
4.Mitral stenosis (MS) :
- Because asymptomatic MS is associated with low mortality, intervention in asymptomatic MS is aimed at reducing the risk of complications (predominantly thromboembolic events) and delaying symptom onset.
- Current guidelines recommend intervention for asymptomatic patients with MS only in the form of percutaneous mitral balloon commissurotomy.
- Intervention in asymptomatic patients with severe MS will remain restricted to rheumatic MS with anatomy favorable for percutaneous balloon commissurotomy among patients who are at high risk of thromboembolic events or hemodynamic decompensation.
5.Primary mitral regurgitation (MR) :
- Factors identified as predictors of outcome among asymptomatic patients with primary MR include LV size and function, atrial fibrillation, pulmonary hypertension, leaflet flail, and marked left atrial enlargement in the setting of sinus rhythm.
- Current guidelines support intervention in asymptomatic patients with severe MR and LV enlargement or systolic dysfunction (LVEF ≤60%, LV end-systolic diameter ≥40 or 45 mm), atrial fibrillation, or pulmonary hypertension; or if there is a high likelihood of successful and durable repair, low operative mortality, and surgery is performed at a Heart Valve Center of Excellence.
- Published studies support the roles of natriuretic peptides, exercise testing, and LV GLS in the assessment of primary MR outcomes.
- The primary factors in determining whether asymptomatic patients with severe degenerative MR and normal LV systolic function should undergo intervention are the safety, efficacy, and durability of mitral repair; which in turn are dependent on the underlying mitral valve pathology, as well as surgeon skill and program experience. Numerous studies have demonstrated that successful valve repair is dependent on surgeon and center volume.
Article sélectionné et traduit par Dr, El kandoussi Tahar